CODING
In order to maximize your return for your hard work, it’s important to make sure your procedures are coded properly.
We understand the challenges of finding affordable coding resources. PUREDI’s certified coding professionals can help relieve this burden. Claims are scrutinized to confirm proper coding methodology. Medical documentation and operative notes are carefully analyzed to ensure maximum reimbursement. While maintaining a focus on compliance, PUREDI’s goal is to optimize revenue and minimize denials or delays in getting you paid.
OUR SERVICES
End-to-end, managing revenue for medical groups is a full time job. We’ve got it covered.
We know it’s difficult and navigating through a myriad of regulations presents more challenges today than ever before. That’s why we make it easier by staying ahead of the game and managing everything for you.
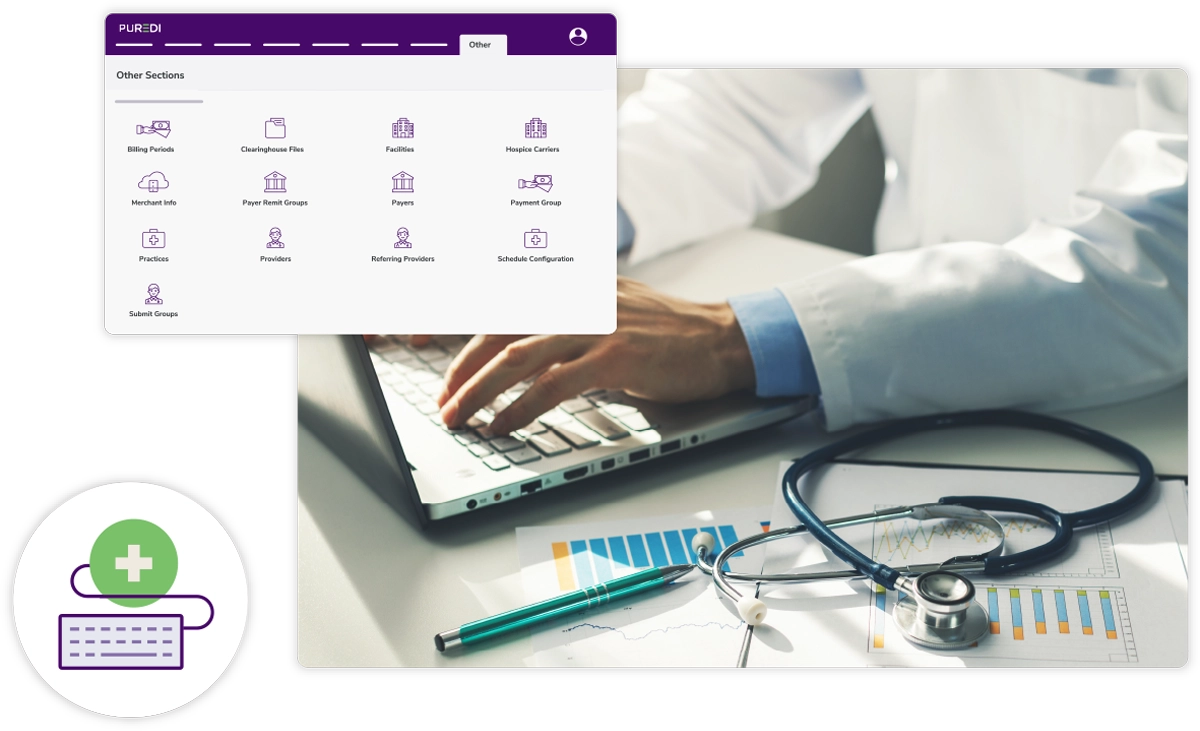
Revenue Cycle Management
Analytics & Reporting
Coding
In order to maximize your return for your hard work, it’s important to make sure your procedures are coded properly.
Practice Management
Connectivity
Credentialing & Contracting
A professional, accurate and efficient contracting process is imperative to efficient medical billing and revenue cycle management.
Recent Blog Posts
Behind the Numbers: How CDI Specialists...
Healthcare team standing together in a clinical environment, led by a nurse in blue scrubs,...
What Is ERA in Medical Billing A Guide to...
Like any other business, cash flow is necessary for healthcare agencies to operate effectively....
A Clinician’s Guide to Navigating Bundled...
The healthcare industry is, as a whole, undoubtedly moving toward value-based care models. As such,...
Medical billing and coding are essential processes in the healthcare industry that ensure providers are reimbursed for their services. Medical billing involves submitting and following up on claims with health insurance companies to receive payment for services rendered by a healthcare provider. Medical coding is the transformation of healthcare diagnoses, procedures, medical services, and equipment into universal medical alphanumeric codes. The coding process involves reviewing clinical statements and assigning standard codes using the classification systems.
The four primary types of medical coding systems used in healthcare include:
- ICD (International Classification of Diseases): This system is used globally to classify diseases and a wide variety of signs, symptoms, abnormal findings, and external causes of injury or diseases.
- CPT (Current Procedural Terminology): This system is used to describe medical, surgical, and diagnostic services and is maintained by the American Medical Association.
- HCPCS (Healthcare Common Procedure Coding System): This system is used for billing a variety of services, including ambulance rides, medical equipment, and certain drugs.
- DRG (Diagnosis-Related Groups): This system is used to classify hospital cases into one of approximately 500 groups, intended to identify the "products" that a hospital provides.
Medical coding can be challenging, as it requires a detailed understanding of medical terminology, anatomy, and the specific coding systems used. Coders must accurately translate complex medical information into standardized codes, ensuring compliance with various regulations and guidelines. The complexity can vary depending on the specialty and the specific requirements of different coding systems. However, with proper training and experience, medical coding professionals can effectively manage these challenges to optimize revenue and minimize denials or delays in getting paid.
Evaluation and Management (E/M) coding is a segment of medical coding that deals specifically with the evaluation and management of patient visits. These codes are used to document the services provided by physicians and other healthcare professionals to assess and manage a patient's health. E/M codes are critical for billing purposes and are determined by the complexity of the visit, the extent of the history and examination performed, and the level of medical decision-making involved. Proper use of E/M codes ensures accurate reimbursement for healthcare providers while maintaining compliance with coding guidelines.




